–
Abstract
Current mental health services across the world remain expert-centric and are based on traditional workflows, mostly using impractical and ineffective electronic record systems or even paper-based documentation. The international network for digital mental health (IDMHN) is comprised of top-level clinicians, regulatory and ICT experts, genetic scientists, and support organizations. The IDMHN has been formed to enable the implementation of digital innovations in clinical practice, hereby facilitating the transformation of current mental health services to be more personalized and more responsive to patients and healthcare needs. This consensus statement summarizes the consortium’s vision and strategy for further development of digital mental health.
1. Introduction
Brain disorders represent key non-communicable diseases of the 21st century: one in four people in the world will be affected by mental or neurological disorders at some point in their lives. Around 450 million people currently suffer from such conditions, placing mental disorders among the leading causes of illness and disability worldwide [Citation1]. Mental disorders have a large impact on individuals, families, employers and communities, and have already surpassed other non-communicable diseases, such as cancer or diabetes, in terms of social and economic burden. Global costs associated with mental disorders were estimated to be €2.2 trillion in 2010 and are expected to rise to €5.3 trillion by 2030 [Citation2]. Mental disorders rank as the main cause of years lived with disabilities (YLDs): four of the six leading causes of YLDs are due to mental disorders, including depression, alcohol-use disorders, schizophrenia and bipolar disorder [Citation3]. People with mental disorders also have a two- to four-fold risk of premature mortality, with a life expectancy that is on average 25 years shorter than that of the general population [Citation4].
Mental health is the main medical area in which decision making for diagnoses and treatment choice is primarily based on clinical interviews, observations and self-report measures. For the majority of mental disorders, no biomarkers or technical tools have been validated to determine diagnosis or propose the most suitable treatment plan. The lack of useful indicators beyond checklist diagnostic criteria is one reason why mental disorders are often misdiagnosed, especially on initial presentation, particularly if diagnostic and treatment guidelines are not used systematically. According to recent surveys conducted by GAMIAN Europe and meta-analyses, the misdiagnosis of mental disorders is a serious problem that occurs in both primary and secondary care mental health and in general practitioner settings:
-
Sixty-nine percent of patients with bipolar disorder are misdiagnosed initially by mental health specialists [Citation5].
-
On average, patients remain misdiagnosed for 5.0–7.5 years [Citation6].
-
Only 47.3% of patients with depression are correctly diagnosed by GPs [Citation7].
As a consequence, the global gap between the need for treatment and its provision is large. The median time to receive a psychiatric assessment and appropriate psychotropic medication is between 7 and 30 days in most EU countries, regardless of symptom severity levels [Citation8]. However, in low and middle income countries (LMIC) between 76% and 85% of people with severe mental disorders receive no treatment for their disorder. The corresponding range for high-income countries (HIC) is also high (between 35% and 50%) [Citation9]. In addition, patients with mental disorders have high rates of untreated medical conditions, for example, diabetes (45%), dyslipidemia (88%), hypertension (62%), and smoking (90%) [Citation10].
2. Digital mental health
Digital technologies and a rapidly developing eHealth field together offer novel opportunities to support and improve mental health services, including the use of internet-based interventions and smartphone applications that address the prevention, treatment and aftercare of mental health problems. With economic pressure on mental health services increasing, e-mental health systems could bridge treatment gaps, reduce waiting times for patients, and deliver interventions at lower costs. The number of mobile health (mHealth) apps focused on mental health has rapidly increased; a 2015 World Health Organization (WHO) survey of 15,000 mHealth apps revealed that 29% focus on mental health diagnosis, treatment, or support [Citation11]. Nevertheless, despite the increasing evidence base for the utility of such interventions, the transition and implementation of these into clinical practice is remarkably slow [Citation12]. For example, in the UK, only two computerized interventions for mental health problems are recommended in clinical treatment guidelines (i.e. ‘Beating the Blues’ for depression, ‘Fear Fighter’ for panic and phobia) [Citation13,Citation14]. Hence, it appears that amongst healthcare providers and potential service users there are barriers to the implementation of effective computerized interventions that have not yet been fully identified or addressed. The results of a recent study suggest that individuals are well aware of the potential advantages of computerized or digital interventions, but may not place particular importance on these factors [Citation15]. This study highlights the need to raise awareness amongst clinicians and service users (most likely via these clinicians) about the growing evidence base for digital (including mobile) mental health interventions. However, several factors, including poor usability, lack of user-centric design, concerns about privacy, lack of trust, unhelpful in emergencies, were suggested as potential contributors to low engagement with mental health apps among the patients [Citation16]. For e-mental health to have the large public health impact that is often anticipated, there is need to improve the translation of eHealth research into clinical practice. Steps towards achieving this not only include improving awareness in clinicians and public, but also increasing the inclusion of information on the evidence-base and efficacy of digital mental health interventions into clinical treatment guidelines. The other pathway to improve user engagement with mHealth solutions for mental health is to involve end users in the conception, design and testing of apps [Citation16].
3. DocuMental
DocuMental is a clinical decision support system (DSS), developed by Documental Ltd (www.documental.ee) in collaboration with eHealth organizations (EIT-Health: European Institute of Innovation & Technology; Estonian Connected Health), the University of Tartu, and the Tallinn University of Technology. The system is purposefully designed for diagnosis, treatment and management of mental disorders, thereby providing a platform for digitized clinical workflows in mental health. DocuMental is a secure, web-based software tool designed for mental health service staff, including physicians, nurses, psychologists, social workers, care-coordinators and healthcare managers. In order to improve user friendliness and clinical workflows, DocuMental’s leading principle is to deliver ‘immediate results’. This aim generates added value: every step forward is associated with results (automated documentation, increased time-effectiveness, process and progress overview, accuracy, error avoidance, confidence, evidence-based data, etc.). To assist mental health service, and patient as well as public needs, ultimately resulting in better outcomes, Documental Ltd has developed and digitized the following modules to date:
-
Diagnostic module: consists of digitized, structured ICD-10 diagnostic criteria and ‘tick mark’ choice questionnaires for all mental health disorders (From F00 to F98), including adult, adolescent and childhood disorders. The ICD-10 diagnostic questionnaires are linked to DSS algorithms, which provide diagnostic suggestions to increase diagnostic accuracy and allow for diagnostic verification and differentiation.
-
Treatment module: consists of the whole list of psychotropic medications, including antidepressants and antipsychotics, registered in the EU for mental health disorders, and operates via DSS algorithms for medication- and treatment-plan selection, including doses and regimens, drug-drug interactions in accordance with widely recognized treatment guidelines. The treatment module is linked to the diagnostic module and tracks medication choices in full accordance with clinical presentation and diagnosis, which helps clinicians to avoid mistreatment and manage care plans in a standardized way. In particular, the DocuMental treatment module provides clinicians with a list of psychotropic medications available in the EU, guides them in their medication choices based on patient diagnosis and presentation, and provides treatment plans in accordance with treatment guidelines.
-
History and routine assessment modules: in order to contribute to standardized and digitizing clinical workflows in mental health, DocuMental has also digitized, structured and automated history and assessment modules for comprehensive personal and family history, mental status, physical examination, risk assessment, and optimal sets of available clinical scales. These modules help clinicians to perform comprehensive and standardized assessments, which is an essential requirement for improving disease management and personalized care.
DocuMental was selected by EIT-Health as one of 21 finalists of Business Plan Aggregator 2016 among digital health innovations and it was the only finalist in the mental health sector. Recently, DocuMental has received an Estonian-Finnish Quality Innovation Award 2017.
4. International digital mental health network (IDMHN)
Mental health systems worldwide, in their current traditional approach, have not yet adequately responded to the need for more precise and personalized diagnosis, treatment and management of mental disorders. To close this gap, we formed an international network for digital mental health comprising top-level clinicians, regulatory and ICT experts, genetic scientists, and support organizations with longstanding experience and highly recognized expertise in mental health, e-health infrastructures and decision support systems. The first joint effort of IDMHN was to verify and confirm the consistency of ICD-10 diagnostic criteria for mental disorders incorporated in DocuMental with the original document. Through this validation step, the IDMHN’s clinical experts aimed to confirm that DocuMental has properly implemented ICD-10 diagnostic criteria as the ‘gold standard’ for mental disorders, and can transfer them into routine clinical practice. The clinical experts of IDMHN have also reviewed other modules of DocuMental, including digitalized questionnaire for mental status examination and pharmacological register for treatment of mental disorders. All clinical experts evaluated web-based DocuMental application via personal access and reported their feedbacks to the consortium. As they concluded, the diagnostic criteria within DocuMental and diagnoses verified by this DSS are in full accordance with ICD-10 original content and diagnostic guidelines. Only minor comments were made about structure and small divergences in some questionnaires. All necessary changes and additions were completed and synchronized with ICD-10 standards and expert recommendations in the updated DocuMental version. Generally, the clinical experts of IDMHN have found that DocuMental ‘is well-arranged, well-engineered and user-friendly application; its diagnostic checklists are in accordance with ICD-10 diagnostic criteria; it contributes to more accurate and targeted diagnosis, and to accelerate the differential diagnosis process; platform is intuitive, comprehensive and user-friendly in order to conduct a complete mental status assessment; implemented medication register connected to prescription option is well applicable for clinical practice and helps rapid orientation in the correct determination of treatment, i.e. clinical rules’. After this first collaborative task, the members of IDMHN developed the current ‘manifesto’ to summarize the consortium’s vision and strategy for further development of digital mental health. There is an urgent need to improve mental disease management and provide more precise and personalized approaches towards better outcomes in mental health. To achieve this goal, current mental health services and care should be dramatically transformed and integrated with novel technologies and facilities. So far, several attempts have been made but have been restricted to research settings; further, only some aspects of mental health have been targeted, and it has taken a long time to prove the concept, which still lacks broad implementation in routine practice. For the first time, a synergistic, multidisciplinary, worldwide consortium have joined forces to establish a trusted, standardized and widely accepted approach for personalized mental healthcare in routine practice and a digitized clinical workflow based on highly promising and innovative solutions. The main ambition of IDMHN is to become the widely recognized lead in digital mental health, to be more proactive in terms of connections with other medical areas, and to be more responsive in terms of collaboration with authorities and organizations which represent the interests of people with mental disorders and psychosocial disabilities. The breakthrough strategy of IDMHN is in coupling of existing clinical standards, genetic advantages and digital innovations, which should result in improved, effective, integrated and responsive mental healthcare by establishing new clinical processes and new clinical pathways in mental health and by enabling the implementation of personalized approaches in practice.
5. The IDMHN manifesto
-
Current mental health services across world are still based on traditional workflows, mostly using nonfunctional electronic record systems or even paper-based documentation. For example, according to a recent survey conducted by University of Tartu at 17 clinical sites in 12 EU countries: two sites are still paper-based only, 11 are using electronic health records (EHRs), and four are using a combination of paper-based documentation and EHRs. All clinical sites recognized that EHRs in their current form suffer from several limitations that hinder their ability to meet patient needs and service demands. In particular, current EHRs lack decision-making functionality, are not user-friendly, are time-consuming with regard to data recording, have poor interdisciplinary transferability, and suffer from insufficient data quality and a resistance to meaningful data tracking and searching. Based on this preliminary survey, it appears that these limited functionalities are perceived by users as a serious disadvantage in terms of data search, overview, analyzing, transmission as well as making appropriate and informed decisions for diagnosis and treatment of mental disorders. Moreover, the lack of a system that can track the quality of a service aggravates insufficiency in resources and contributes to ineffective service distribution.
-
Despite the availability of reliable and widespread clinical descriptions, diagnostic guidelines and genetic biomarkers included in clinical guidelines (e.g. Clinical Pharmacogenetic Implementation Consortium) and drug labeling, rates of adherence among clinicians to these standards remain low. One of the most serious barriers to their utilization, beside nonfunctional EHR and paper-based documentarians, are time limitations, insufficient human resources and ‘expert-centric’ attitudes. Mental health practitioners are required to undertake interviews, e.g. personal, family and health history, and conduct comprehensive assessments, e.g. mental status, physical health, risk assessments and clinical scales, to reach the most appropriate decisions for a possible diagnosis and treatment plan, all within short consultations (about 45 min for first contact and 15 min for follow-ups). As a result, very high caseloads and time pressure may contribute to lapses in history-taking, potential medical errors and unreliable treatment decisions. The other challenge faced by all countries is scarcity of specialist human resources. The number of specialized and general health workers dealing with mental health is grossly insufficient. Globally, the median number of mental health workers is 9 per 100,000 persons, but there is extreme variation (from below 1 per 100,000 population in LMIC to over 50 in HIC) [Citation17]. Pressure on resources across public services creates a powerful incentive for developing new ways of delivering care and support. Meeting rising demand and ensuring that more people have access to treatment and support are significant future challenges for the mental health sector. In contrast to any other medical area, where diagnosing and treatment plan are based on highly sensitive and specific tests and technical innovations, psychiatry is still positioned as a ‘medical art’, in which initial clinical impressions that are made by professionals usually during first interview or observation of a patient, often predetermine final decision in terms of diagnosis and treatment choice. The digital innovations bringing diagnostic and treatment standards into clinical practice and increasing patients and their representatives’ involvement in care plans would transform current mental health services to be more ‘patient-centric’ and assure the improvement of service quality via tracking systems following compliance with required clinical and psychosocial standards for patients’ needs.
-
Public expectations of mental health services, and how they might interact with them, are changing. Through greater use of technology, the public are becoming more engaged and better-informed consumers of their own healthcare. By making the most of the opportunities presented by e-mental health and digital innovations, we can address some of the biggest future resource challenges facing the mental health sector – for example, the costs of service delivery, workforce issues, access to services and continuity of care. As traditional approaches struggle to meet this overwhelming need, new technologies are required to expand access and improve health outcomes at lower costs. Our firm belief is that quality improvement in mental health services, including their ability to provide support and effectively complete their responsibilities for identification, prevention and management of mental disorders, would significantly improve if the highest international standards and instruments orientated on achieving better outcome, health recovery and human rights protection are digitalized and implemented in everyday practice. This would be performed via existing e-approaches, including electronic record systems, online-based applications and mobile apps, particularly those facilitating shared therapeutic decisions between clinicians and service users. Achieving this goal is crucially dependent upon assuring that mental health services routinely use the same standards when providing treatment and support to people with mental disorders and psychosocial disabilities or needs.
-
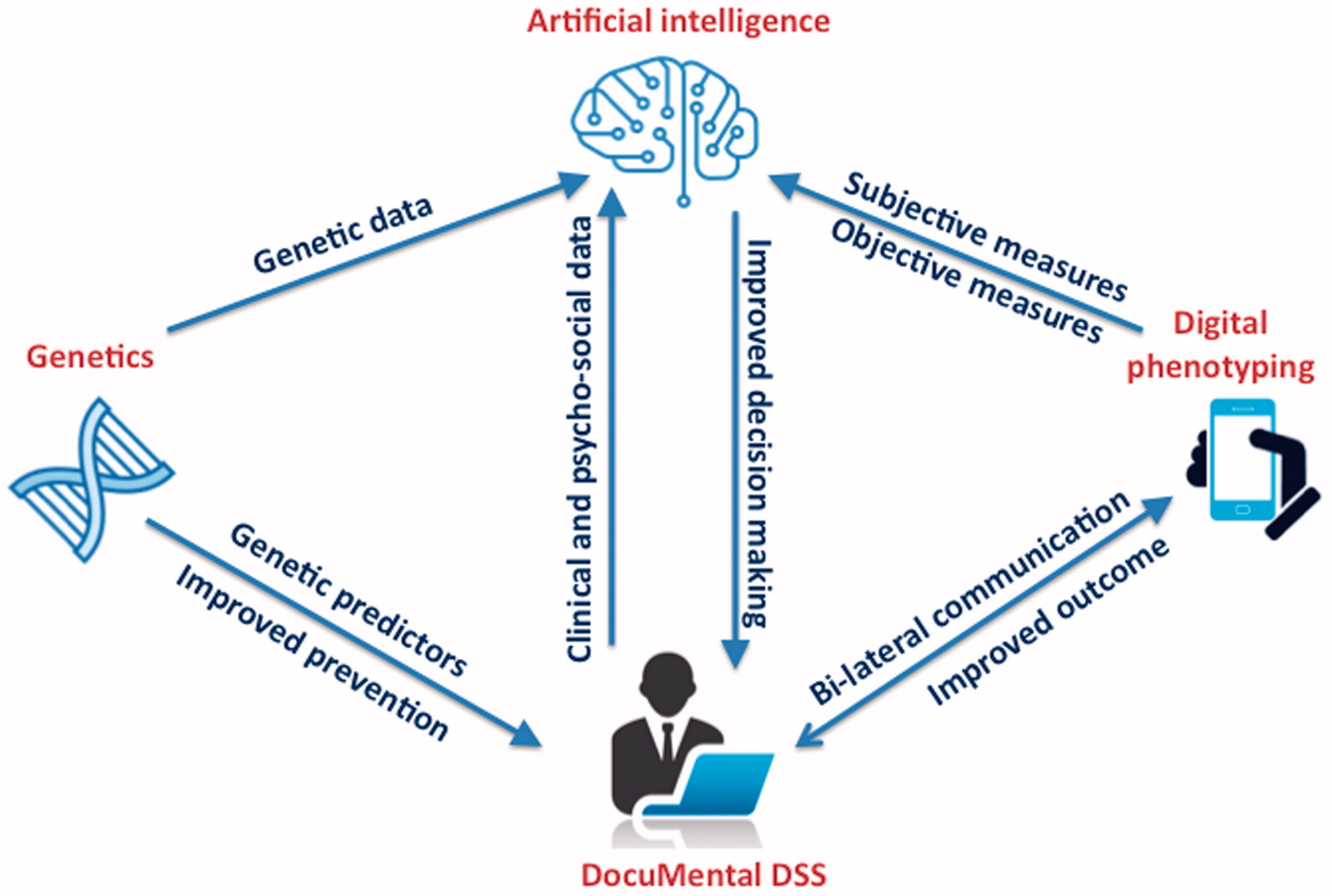
The new concepts contributing to more precise and personalized mental healthcare through the integration of IT innovations, digital phenotyping, genetic approaches and cloud-based facilities and technologies should improve the management of mental disorders. The main benefit of such an approach is the expected shift of current, traditional mental health practices towards preventive healthcare based on proactive assessment and screening programs combined with early intervention and treatment, instead of reactive disease treatment, and, as result, a reduced burden on patients, their social communities, and their healthcare systems. The current IDMHN consortium has proposed the joint action for development of cloud-based Intelligent Platform for Research, Outcome, Assessment and Care in Mental Health (i-PROACH) enabling the wide implementation of standardized clinical processes and pathways in mental health. We believe i-PROACH will be established as a new internationally trusted tool for addressing societal needs for more precise and personalized diagnosis, treatment and management of mental disorder through its innovative solutions, including clinical DSS (DocuMental software), algorithms on genetic data (as provided by Biobanks and genetic initiatives, for example U-PGx: Ubiquitous Pharmacogenomics http://upgx.eu/), digital phenotyping and artificial intelligence tools (). In particular, the i-PROACH platform should promptly lead to patients receiving more standardized and evidence based care plans, less complications and less comorbidities whilst reducing treatment cost by avoiding unnecessary or incorrect treatment medications, and provides transparent data for monitoring and measuring outcomes, quality of care and services provided. By facilitating the further integration of the i-PROACH platform and its individual components with other evidence-based technologies (genetic test, neuroimaging, blood analyses etc.), the future development of personalized medicine approaches in mental health will be also supported in the long-term.
-
There is increased trust in cloud-based infrastructures among healthcare providers and increased awareness that existing infrastructures within healthcare services are insufficiently flexible for changes and lack necessary functionalities to address current challenges with data quality and data exchange. In particular, the quality, access and interoperability of existing data collected via the majority of EHRs in mental health are far from ideal, due to several limitations and barriers. Generally, these data are not structured, not trackable, content-poor, and lacking in standards and indicators. Several European initiatives, for example BBMRI and ELIXIR, facilitate utilization of shared infrastructures and services, and provide data management technologies in open cloud-based environments, which contribute to reusable and quality data and meaningful analytical value in mental health, especially if data are collected in standardized and well-structured way. More attention should be paid to high-quality (digitized and standardized), reusable (interoperable and real-time updated), and large multidisciplinary (e.g. clinical, demographic, psychosocial, digital phenotyping, genetics) data collection, handling and access in international mental healthcare and services. It also requires compliance with regulatory processes, including data safety, privacy protection in line with the General Data Protection Regulation (GDPR) requirements and Digital Single Market policies, where appropriate. As the first stage, we are planning to elaborate the strategy for processing data to European Open Science Cloud (EOSC) services to enable the i-PROACH implementation process when integrating the i-PROACH platform with existing e-infrastructures and cloud-based environments across EU countries. We will establish dialog between actors involved in official agreements and resource allocation and proceed with legalization processes to enable the integration of i-PROACH with healthcare databases and systems; data hosting at local data storage services and further transfer of research data (anonymized or de-identified) to i-PROACH cloud.
-
Access and integration of health-related data from multiple sources create unprecedented opportunities for increasing the quality of healthcare by generating, integrating and managing health data from heterogeneous sources when healthcare providers are enabled to share part of their data with the different stakeholders involved in the provision of health services to patients. The important issues in the i-PROACH project regarding the GDPR are principles for processing personal data, especially health-related data, consent management and anonymization, accountability and data governance, data protection by design and default, data exchange, security measures and data processors. We will analyze the impacts of these issues on the digitalization of health professionals’ workflows and sharing of sensitive data across the EU, and will explore security mechanisms like blockchain and new anonymization models like controlled access and implement solutions which enable the management of information privacy and trust in the networks accordingly to the GDPR principles. We also aim to establish a data management plan (DMP) to present rules and guidelines for the management of personal sensitive and non-sensitive data and ensure compliance with European and national regulations including data security ethical issues. To support the data management and processing within the i-PROACH platform, we intend to develop secure cloud-based solutions, allowing users to run applications processing sensitive data in a secure environment. It would facilitate collecting international or cross-border data into the same data catalog with access to secure processing environment, supporting efficient large analyses, required for research and administrative evaluations.
-
In the context of improving access to care and service quality, WHO recommends the development of comprehensive community-based mental health and social care services; the integration of mental health care and treatment into general hospitals and primary care; continuity of care between different providers and levels of the health system; effective collaboration between formal and informal care providers; and the promotion of self-care, for instance, through the use of electronic and mobile health technologies [Citation9]. A substantial and increasing proportion of people with mental disorders are being seen by GPs or in community-based settings and in private practice. All of these areas lack specific digital platforms for mental health. We thus aim to provide comprehensive, integrated and responsive mental health services in community-based and primary care settings. This can be achieved by integration of the i-PROACH platform with social and primary care services and by providing support to increase confidence and skills among non-specialized health workers in recognizing and managing mental disorders. The i-PROACH platform may contribute to shifting the focus of care away from long-stay hospitalization in mental-health institutions towards non-specialized health settings, with increasing coverage of evidence-based interventions (including the use of stepped care principles, as appropriate) for priority conditions, and using a network of linked community-based mental health services (including short-stay inpatient care, and outpatient care in general hospitals, primary care, comprehensive mental health centers, day care centers) to support people with mental disorders living with their families and in supported housing. This strategy will facilitate the resource savings and reorganization of mental health services by reducing administrative, human and time-related costs, and improving management and care plans, including hospitalization length and number of visits.
-
The i-PROACH platform may provide unique opportunities for clinical research and scientific programs and contribute to increased research activity at local, national and international levels in mental health, particularly due to international standards, and support data-searching facilities and possible interconnectedness with other interdisciplinary technologies. In line with the Mental Health Action Plan 2013–2020 [Citation9], i-PROACH may contribute to improvements in research capacity and academic collaboration on national priorities for research in mental health. In particular, the i-PROACH platform is designed to collaborate with existing research projects, such as PerMed for the implementation of systems and personalized medicine in Europe, the European Alliance for Personalized Medicine, and international organizations, such as the Global Alliance for Genomics and Health and the BBMRI and ELIXIR bioinformatics infrastructures, in order to ensure maximal impact. Furthermore, by accumulating large quantities of detailed data about individual patients and through the development of genetic and predictive models, the i-PROACH may also support initiatives of biotechnology partners to collect comprehensive data on the safety, efficacy, and effectiveness of innovative medicines, and the development of new, personally ‘tailored’ drugs. Due to the standardized and digitized clinical workflow in mental health across worldwide countries we will also facilitate real-time search of potential patient participants for research studies, which should reduce costs and increase feasibility in practice. Overall, i-PROACH will conduct research in collaboration with multidisciplinary teams with expertise, resources and research capacities to achieve the critical mass needed to complete the expected research and move towards the common goal of promoting the preservation of health and preventing the onset of disease. We also aim to expand i-PROACH’s involvement in scientific and academic activities to become the most powerful, international platform for the promotion of research in mental health and for the more effective use of necessarily limited resources. The i-PROACH platform also aims to support equity for countries with low or middle income in obtaining resources, and to secure their involvement in research and consortium programs.
-
Mental health strategies and interventions for treatment, prevention and promotion must be based on scientific evidence and best practice, and therefore should implement the principles for more precise and personalized approaches in routine management and care of mental disorders. To achieve this goal, we are aiming to establish a process of scientific validation for e-mental health innovations, including i-PROACH platform considering the following sequence before full implementation: Feasibility/Pilot (Evaluating retention/acceptability, safety, satisfaction) followed by a Randomized Controlled Trial either against treatment as usual or a non-inferiority trial vs. an evidence-based intervention. An implementation feasibility study could be the final part of the process in order to assess large-scale feasibility. Furthermore, the improvements in mental disease management and mental healthcare outcomes that result from the transformation of traditional models of care, patient journeys and clinical pathways to the new personalized and predictor-based digitized clinical workflows should be evaluated by applying health impact and the cost-effectiveness analyses. This is particularly important considering the considerable social and economic burden due to mental health disorders. As the first pilot the economic impact of implementing personalized mental health approach provided by i-PROACH will be evaluated in Estonian healthcare systems (). With the Estonian National Health Information System (ENHIS) in place (used by all Estonian healthcare providers, who are obligated to forward medical data to ENHIS), innovative programs towards personalized medicine, a national digital prescription system, and an established state-of-the-art genome center, Estonia, with its modern and relatively simple health system, is particularly suitable to pilot i-PROACH in routine clinical practice and implement it fully on a national scale. During this pilot, we will be able to demonstrate and establish interoperability between i-PROACH platform and existing healthcare systems, including EHRs, ENHIS, the patient portal, digital prescriptions and the Estonian Biobank; and to elaborate models for 1) health impact analysis: based on direct patient level outcomes (such as relapse rate and quality of life within-normal) and indirect indicators (such as hospitalization length, re-admission/presentation rates), and 2) the cost-effectiveness analysis: based on direct costs of using healthcare services, costs for developing, implementing and maintaining digital solutions, and costs for training healthcare staff.
-
Despite the prioritization of mental health by the WHO as medical area which requires more attention and transformation, this field is still significantly less funded by grant resources, such as European Commission or EIT-Health, than, for example, oncology or cardiology. Psychiatric consortia aiming to bring innovations into mental health often face questioning attitudes in experts involved in application review. This is reflected by the low number of successful and funded projects on digital mental health led by psychiatrists. The project revision systems need more transparent and fair approaches, with better opportunity for bilateral feedback and communication on individual projects. As recognition of this problem, EIT-Health recently made a very significant step towards improvement in their evolution process of submitted applications by increasing decision based on project face-to-face hearing rather than based on remote expert review. Such changes give more chance to research teams to explain project details in better way than it might be done in writing form. Our multidisciplinary consortium has the required skills and expertise through world`s leading scientists in clinical research and ICT/eHealth to explore and exploit innovations and strategies for digital personalized mental health. We are confident that i-PROACH will improve personalized mental health and care beyond the current ‘state-of-the-art’ – it is ambitious, but also realistic and achievable. To increase recognition of our consortium and its potential in innovation and research for mental health, we will establish closest possible collaborations with key stakeholders in healthcare and promote our vision through proactive involvement in calls and actions related to digital and personalized medicine.
-
Due to digitalized and integrated international standards for assessment and treatment of mental disorders, i-PROACH represents a promising tool for teaching, education and revalidation of mental health workers and medical students. In particular, we aim to implement education activities tailored to the needs and interests of the target groups. The activities would include: (1) consortium website: to provide the results of the i-PROACH progress, information about upcoming conferences the IDMHN will attend, and available publications; (2) policy events: to increase collaboration with authorities and policy makers, etc., (3) peer-reviewed publications: to facilitate the distribution and uptake of i-PROACH results; (4) presentations at conferences: to present research results at established international conferences by professional societies; (5) guidelines: we plan to develop i-PROACH guidelines to guide clinicians in preventing certain outcomes, such as relapse, somatic risks, adverse side effects of drugs, drug-drug interactions, etc. by using platform. Planned educational materials will be available to all interested parties through the website. The following training activities to facilitate the innovation and implementation of i-PROACH for personalized mental health will include: (1) i-PROACH User Manual; Tutorials; and Videos; (2) i-PROACH online training: we aim to design an online training class consisting of modules based on the most common user activities of the i-PROACH platform. Healthcare providers would be able to sign up for free and try out the different functionalities without having an implemented platform available in their institution. This will help future users to prepare for the implementation of the platform in their work and will also help interested future users to get a feel for how the platform may positively influence their clinical workflow. Furthermore, the service users involvement (PPI) in the further development and implementation of i-PROACH platform will be also encouraged in order to optimize the acceptability.
-
To maximize the impact of the i-PROACH project we will establish strategy based on stakeholder involvement and target-group orientation, including patient representatives, particularly GAMIAN, authorities and policy makers, etc. The proposed target-group orientation will allow us to define and implement measures geared to the specific needs of the different groups. The i-PROACH platform will implement dissemination activities tailored to the needs and interests of the target groups. As the main focus of dissemination is on the distribution and uptake of results, most activities will focus on the scientific community, healthcare providers and policy makers. Through an established international network, we will introduce i-PROACH solutions to key stakeholders and thus to expand engagement with our project. In particular, the members of team and partners are involved in scientific and management boards at several international organizations and thus may help to maximize the visibility of i-PROACH project and platform to broad audience. We also aim to increase collaboration with patients, authorities, professional organizations (such as European Psychiatric Association, World Psychiatric Association, World Federation of Societies of Biological Psychiatry, World Congress on Medical Informatics and others), policies makers, eHealth experts in plans and strategies for i-PROACH. The eHealth and ICT-oriented technology and business meetings will also help to introduce the platform and facilitate contact with potential major industry and investors. We aim to develop a detailed plan for horizontal and vertical knowledge dissemination, to ensure that awareness of the i-PROACH project is disseminated widely and freely available among local and international stakeholders, including governmental and non-governmental organizations, commercial companies, researchers, clinicians, policy makers and the public. Additionally, in close collaboration with European and national medicine agencies the IDMHN also reviews and adjusts the list of medications registered for mental health to their local availability in order to aid the adequate choice of medicines via i-PROACH platform for each involved country.
-
Digital solutions have the potential to reorganize current healthcare systems by bringing new services, influencing policies impacting personalized healthcare approaches, and developing reimbursement that would be favorable for the implementation of personalized medicine. Conversely, such strategy in mental health would prevent numerous serious adverse events and thus save resources, which will lower the costs of the respective healthcare systems. The complexity of the scenario requires thorough health economical evaluations, such that the results of i-PROACH would not only provide conclusive evidence of improved patient outcomes but also document simultaneously the costs of healthcare. Thereby, i-PROACH should further facilitate the incorporation of personalized health care measures into national and international guidelines and change clinical practice. The economic impact of i-PROACH is potentially huge – early identification of at risk individuals (prevention of disease), personalized approach and increase adherence to intervention, early and effective treatment will reduce burden of disease, complications associated with chronic diseases as well as related treatment and hospitalization costs, thus reducing the burden of morbidity and mortality to society. For example, a Danish randomized controlled trial of CYP2D6/CYP2C19 found that pharmacogenetic testing in patients with schizophrenia significantly reduced costs among the extreme metabolizers (poor metabolizers and ultrarapid metabolizers), including costs of psychiatric care, primary care services and pharmaceuticals. This study demonstrated an excess of costs in extreme metabolizers ranging 177–239% higher than ‘normal’ metabolizers; when using genotype-guided treatment, however, this excess cost was reduced by 23–48% [Citation18]. In addition, a recent multicentre, randomized controlled trial showed that compared with usual care, an intervention based on personal predictors of risk of depression implemented by GPs is a cost-effective strategy to prevent depression [Citation19]. Thus preliminary evidences of cost savings provides further support to the implementation of digital solutions into clinical guidelines and practice. Therefore, the detailed cost-effectiveness analyses will also need to convince health insurance companies and related organizations to reimburse and support the clinical application of the new strategy and digital innovations in mental health. Considering that i-PROACH platform potentially has a very broad implementation range, covering different ‘market areas’ and involving a diverse community of users, it must also be competitive priced and qualify for the same level of reimbursement. In particular, the business scheme for DocuMental is planned as a subscription-based licensing model, where price calculation will take into account the number of users, utilization of services, regional economic conditions, copyrights and permission expenses, upgrades, technical support and profit. However, the main principle of DocuMental and other licensed components of the i-PROACH platform is in immediate value for mental healthcare and users, where expenses on subscription of digital innovations should be significantly less than total outcome and benefits raised by their implementation in everyday clinical practice.
6. Summary
It is widely recognized and generally accepted that existing standards for identification and management of mental disorders, including diagnostic and treatment guidelines as well as polices for human rights protection should be applied and strictly followed world-wide. The current international consortium aims to implement i-PROACH principles into everyday practice within a range of geographically and socioeconomically diverse countries in order to improve identification, management and prevention of mental disorders via digitized and personalized approaches, and to contribute to overall improvements in mental health services. The breakthrough approach of i-PROACH is in coupling these standards and eHealth innovations, which results in improved, effective, integrated and responsive mental health sectors through enabling the implementation of standardized instruments in practice. This approach has a high potential to address current needs in mental health, to become more transparent in terms of service access and quality, to be more beneficial in terms of outcomes and burden reduction, more proactive in terms of connection with other areas, and more responsive in terms of collaboration with authorities and organizations representing the interests of people with mental disorders and psychosocial disabilities.
Disclosure statement
Prof. Eduard Maron is the founder and CEO of Documental ltd. Prof. Siegfried Kasper and Prof. David Nutt are members of advisory board of Documental ltd. None of these advisors or other members of the IDMHN, expect of EM, have shares in Documental Ltd. This manifesto was developed by joined effort of IDMHN based on the best interest for mental health area and public under fair and professional principles.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Link: https://www.tandfonline.com/doi/full/10.1080/2575517X.2019.1617575
